
Education
- IRIS Staging System
- Risk Factors for CKD
- Early Diagnosis of CKD
- Creatinine (Dog)
- Urine Collection
- Urine Specific
Gravity - Proteinuria
- Hypertension
- GFR
- GFR in Practice
- Preventing Aminoglycoside-induced AKI
- Treatment of
Vomiting, Nausea and Inappetence in Cats with Chronic Kidney Disease - Diets for Cats with Chronic Kidney Disease
- Reassessment of "Normal" Values in Dogs and Cats with Chronic Kidney Disease
- Differentiation
between Acute Kidney Injury and Chronic Kidney Disease - Recent advances in Mineral and Bone Disorders in CKD
- Utility of Creatinine, UPC, and SDMA in the Early Diagnosis of CKD
- Inhibition of the
renin-angiotensin-aldosterone system in cats and dogs: The emerging role of angiotensin II receptor blockers - What pet owners should know about kidney function and the diagnosis and management of chronic kidney disease in dogs and cats
- Pyelonephritis
- Renal Biomarkers
- Hypercalcemia in
CKD - A review of the role of fibroblast growth factor 23
Creatinine (Dog)
Interpreting blood creatinine concentration in dogs (revised 2022)
R Heiene, Oslo, Norway
Where does creatinine come from?
Creatinine is produced in vivo by an irreversible, non-enzymatic process. This occurs at an almost constant rate, such that about 2 % of the body's creatine and phosphocreatine pool (mostly present in muscle) is converted to creatinine each day. Once it reaches the blood stream, creatinine is filtered freely by glomeruli and is neither reabsorbed nor secreted significantly by renal tubules.
Why is blood creatinine measured?
The main reasons are to detect and/or monitor acute kidney injury (AKI) and chronic kidney disease (CKD).
What does an increase in blood creatinine concentration indicate?
The concentration of creatinine in blood (i.e. in either plasma or serum) is principally interpreted in relation to renal elimination. When renal function decreases beyond a certain point, an increase in blood creatinine concentration (hypercreatininemia) ensues, usually accompanied by increased urea concentration. "Azotemia" refers to an increases in either or both of these analytes, but the focus here is on creatinine, because of its central role in the IRIS protocols for Staging CKD and for Grading AKI.
Although hypercreatininemia occurs with substantial renal dysfunction, some other possibilities have to be considered as well, because moderate hypercreatininemia could also be related to:
- High muscle production of creatinine, especially in dog breeds with large muscle mass, such as boxers, greyhounds, sled dogs, etc.
- Reduction in extracellular fluid volume: dehydration may increase blood creatinine concentration when dehydration exceeds 5%.
- Intestinal absorption of exogenous creatinine (some creatine in meat is converted to creatinine during cooking).
What are the optimal analytical conditions?
- Serum vs. plasma: Creatinine concentrations are similar in serum and plasma.
- Storage: Creatinine is stable at 20°C for up to 24 hours in blood without anticoagulant and up to three days in plasma or serum. At -20°C, stability is excellent (at least eight months).
- Analytical interferences: Haemolysis has no effect on blood creatinine. With assays based on Jaffé's reaction (still largely used in human laboratories, but not in veterinary practice), high concentrations of bilirubin, lipids, and glucose may lead to overestimation of blood creatinine concentrations. Cephalosporins may increase blood creatinine values determined by Jaffé's method by up to 50%.
What physiological factors affect blood creatinine concentration?
- Age: Blood creatinine increases during growth in the puppy up to one year. In healthy geriatric dogs, blood creatinine is similar to that observed in young adults.
- Body weight: Blood creatinine increases with the body weight in dogs. Large muscle mass may explain moderately increased blood creatinine concentration. In contrast, muscle atrophy in cachexia may decrease blood creatinine values.
- Breed: Blood creatinine is generally higher in large dog breeds.However, there are wide differences in concentration between dogs of similar size and considerable overlap between smaller and larger dogs (Figure I). In a recent study this effect is also observed in dogs of different breeds.1
(graph reproduced with kind permission of J Aasen, R Heiene, C Trangerud and E Teske)
Figure 1. Creatinine concentration vs. body size in 567 dogs of various sizes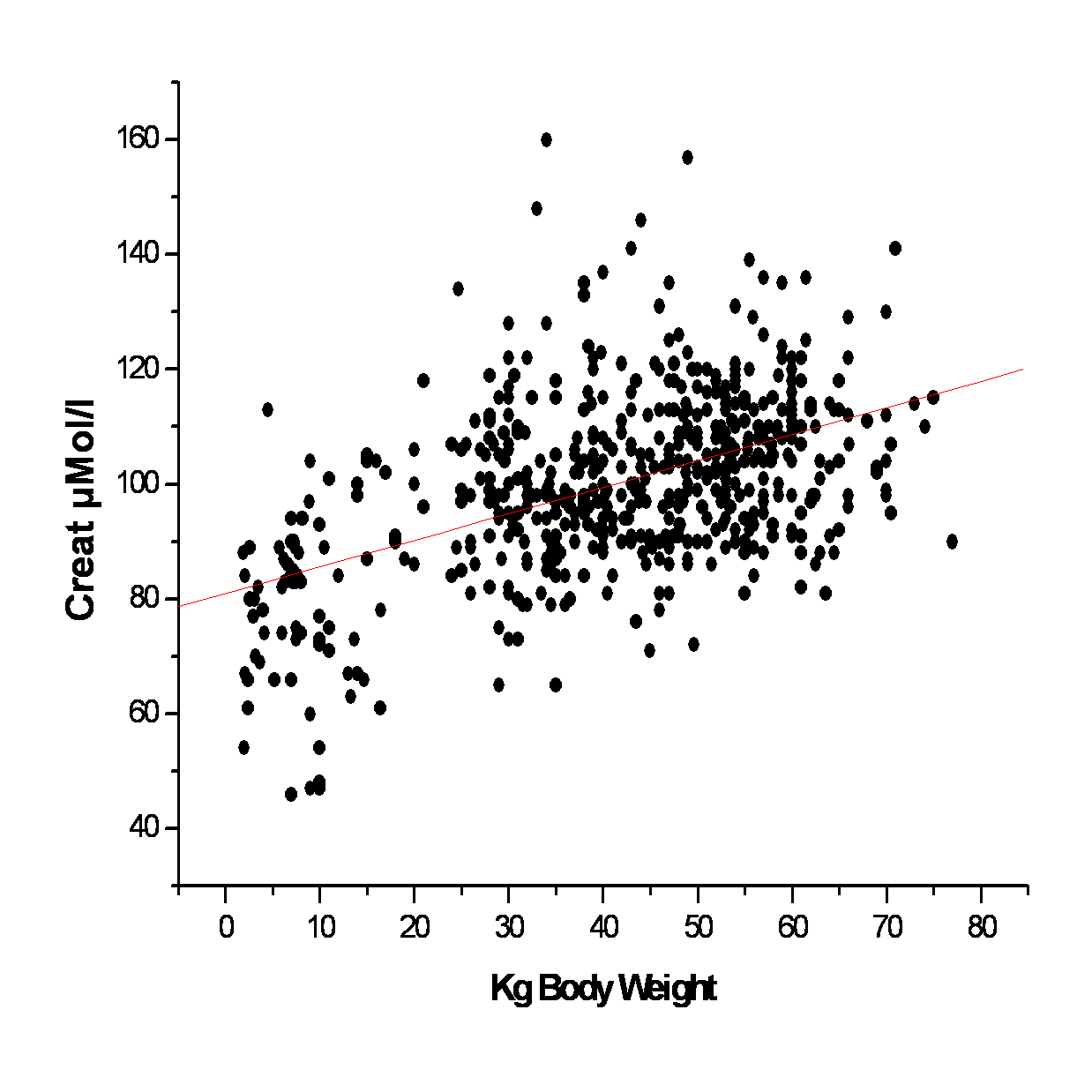
- Time of sampling: There is no known variation in blood creatinine throughout the day in dogs, but the possible effects of meals should be considered (see below).
- Exercise: Exercise may increase blood creatinine concentration in greyhounds (by about 20% in the 60 minutes following exercise), but apparently not in sled dogs. Practically speaking though, an untrained dog can be sampled either immediately or later, after exercise (even if strenuous).
- Feeding: Food intake is a potential cause of variation in blood creatinine concentrations. Increased concentrations (up to 50%) may be observed one to four hours after a meal, especially when cooked meat is given. This increase is explained by intestinal absorption of exogenous creatinine generated from muscle creatine during cooking. It is probably preferable, therefore, to sample the dog in the fasted state (at least eight hours fasting).
Is blood creatinine concentration sensitive in detecting renal dysfunction?
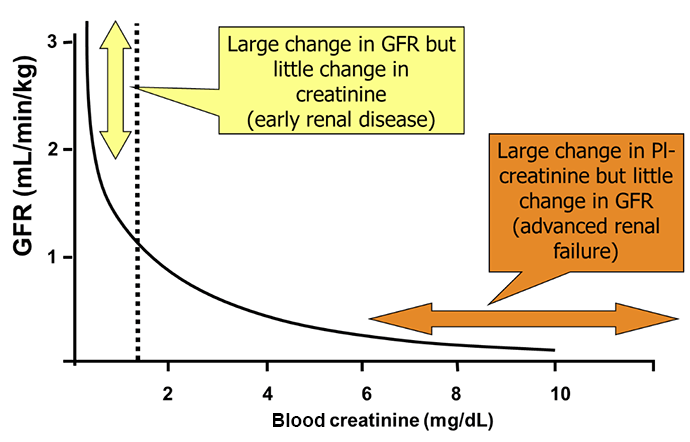
While measurement of blood creatinine concentration is very useful, some limitations have to be kept in mind. In particular, note that the relationship between creatinine and glomerular filtration rate (GFR) is curvilinear (Figure 2), and therefore:
- GFR may decrease rapidly in the early stages of progressive kidney disease without any obvious increase in blood creatinine concentration; or any increase may be small, within the reference range, and so potentially considered to be unimportant.
- In the later stages of progressive kidney disease, even a modest decrease in GFR will lead to a marked, rapid increase in blood creatinine concentration (Figure 2).
Figure 2. Relationship between blood creatinine concentration and GFR:
The use of serum creatinine as a GFR marker has been questioned due to the above mentioned physiological factors influencing it. Alternative surrogate markers of glomerular filtration rate not influenced by muscle mass include Cystatin C and symmetric dimethylarginine (SDMA). These have been suggested to be better performing blood biomarkers of renal function in humans and animals. However, the data in dogs and cat is limited and one recent study indicated that creatinine is not inferior to either Cystatin C or SDMA, when compared to measured GFR in 97 dogs 2
Two different approaches to interpreting blood creatinine concentrations:
- A single isolated value from a given dog can be compared to a reference interval.
This approach is often the only one available, but it is not ideal. Reference intervals have generally been poorly defined on a limited number of animals and can differ greatly between countries and assays. Thus, a decision threshold can neither be transferred from one laboratory to another, nor from published values to your own practice, unless the conditions are identical.
Remember that hypercreatininemia identified from a single sample does not necessarily mean renal dysfunction is present, but it does indicate a need for other testing (urine specific gravity, proteinuria, etc.) to further assess renal function and disease.
- A value obtained at a particular time in a given dog can be compared to another value obtained in the same dog at a previous time.
If conditions are standardized (same assay technique undertaken by the same laboratory, fasted dog, etc), this is probably a better way to monitor renal function over time. An increase or a decrease in creatinine generally indicates a decrease or an increase in renal function, respectively, though any possible effects of reduced muscle mass in cachexia should also be considered (see above).
This approach is particularly recommended in animals with identified acute kidney injury or chronic kidney disease, or to detect early nephrotoxic effects of drugs (though other markers such as enzymuria may be considered more sensitive).
This approach is also recommended when assessing fasting blood creatinine concentrations determined as part of a routine health-monitoring program in older patients.
1. Coyne M SD, Clements C, McCrann 3rd D, Olavessen L. Association between breed and renal biomarkers of glomerular filtration rate in dogs. Veterinary Record 2020;187:ePub.
2. Pelander L, Haggstrom J, Larsson A, et al. Comparison of the diagnostic value of symmetric dimethylarginine, cystatin C, and creatinine for detection of decreased glomerular filtration rate in dogs. Journal of Veterinary Internal Medicine 2019;33:630-639.
Further reading
Braun JP, Lefebvre HP. Kidney function and damage. In: Clinical biochemistry of domestic animals, 6th Edition, Kaneko JJ, Harvey JW, Bruss ML (eds), Academic Press, Burlington, MA, 2008, pp.485-528.
Pressler BM. Clinical approach to advanced renal function testing in dogs and cats. Veterinary Clinics of North America: Small Animal Practice 2013;43:1193-1208.
The previous version was written by HP Lefebvre and ADJ Watson (2015)